
Why Do Runners Get Frontal Knee Pain?
Did you know that when you run you are putting 4-8 times your body weight through your knees!!!
When you consider this statistic it is not surprising that runners frequently develop knee pain. There are many structures that can be affected and areas of the knee that can become symptomatic, however the most frequent is frontal knee pain, or more medically termed Anterior Knee Pain (AKP). In order to understand why this problem occurs it is necessary to have an understanding of the structures and muscle groups that are involved in running.
Anatomy
The Knee Joint
The knee is classified as a hinge joint that is formed by the articulations of the femur (thigh bone) and the tibia (shin bone). The joint is supported by four main ligaments; the lateral collateral ligament (LCL), the medial collateral ligament (MCL), the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). There are two shock absorbing cartilage pads that are situated on top of the tibia known as the menisci. These structures also assist in allowing the joint to move smoothly. The quadriceps and the hamstrings are the two main muscle groups that move the knee joint and provide dynamic support. These structures can all be damaged due to wear and tear and from direct traumatic events.
The Knee Cap
The knee cap is a small triangular shaped bone that sits on top of the femur in a little groove which allows it move as the knee bends and straightens. The purpose of the knee cap is to improve the mechanical efficiency of the quadriceps muscles. This means that they are able to generate more force with less effort. The knee cap has a layer of hyaline cartilage on the back of it which allows it to articulate within its groove with less resistance. The knee cap is held in position by the quadriceps tendon and little ligaments called the coronary ligaments. This is important to know as it allows us to understand, in part, why anterior knee pain may develop in runners.
The Quadriceps Muscles
There are 4 quadriceps muscles; Vastus Lateralis, Vastus Intermedius, Vastus Medialis and Rectus Femoris. The three Vastus muscles originate from the shaft of the femur and Rectus Femoris originates from above the hip joint, with all 4 jointing together to form a strong thick ligament over the patella before attaching into the top of the shin bone. The Quads are a major muscle group involved in running and providing knee stability. The action of the quads is to extend the knee. They are prominent in activities such as walking, running and squatting.
The Hamstring Muscles
The hamstrings are a group of 3 muscles (Biceps Femoris, Semitendinosus and Semimembranosus) found on the back of your thigh that attach to the back of your pelvis and into the top of the tibia and fibula bones. They are commonly injured muscles in all athletes but particularly runners. The function of the hamstrings is primarily to flex the knee and contribute to hip extension. They also provide a key role in stabilizing the knee joint, and help to control the forward movement of the tibia when the free leg is swinging during walking and running to prevent the knee snapping into hyper extension.
The Gluteal Muscles
The Gluteal muscles are actually situated higher up the body around the hip. However they are worth considering as frequently AKP can be traced back to problems with the gluteal muscles. The three gluteal muscles include, Gluteus Maximus, Gluteus Medius and Gluteus Minimus. These muscles have a variety of actions on the hip. They all abduct the hip (lifting the leg out to the side), Glute max extends the hip (lifts the leg backwards) and helps to turn the hip outwards (lateral rotation) and glutes med and min help to rotate the hip inwards (medial rotation). So they have a key role to play in what happens at the hip and therefore have an influence on what occurs at the knee.
Patello Femoral Pain Syndrome (PFPS)
PFPS is the most common diagnosis for knee pain in athletic and non-athletic populations. This condition can essentially be broken down into three forms; knee cap instability, PFPS with malalignment of the knee cap and PFPS without malalignment of the knee cap. This essentially means that there are many mechanisms which can cause PFPS within the knee, which adds to the complexity of the condition and requires a thorough assessment in order to establish exactly what structures and mechanics are causing the problem.
The most likely cause of PFPS is as a result of the knee cap maltracking during knee flexion and extension. Most frequently the knee cap will move laterally due to tight structures on the outside of the knee and a weakness of the inner most quadriceps muscle. In this scenario the tight structures on the outside of the knee will pull the knee cap laterally causing the knee cap to sit just outside of the patellofemoral groove. This can cause irritation to the cartilage that lines the back of the knee cap, causing it to become inflamed. Once inflamed and irritated it can cause the knee cap to become a little bit stuck which increases the chances of it staying in a mal aligned position. It is also believed that when the knee cap is not in the right position that there can be an increased amount of stress placed to the back of the knee cap which can result in pain. Similarly inflammation may occur at the patellar retinaculum (a fascia structure that attaches to the two sides of the knee cap to help to stabilise it) known as a ‘synovitis’.
Symptoms of PFPS include a gradual onset often for an unknown reason to the athlete with vague widespread pain felt over the front of the knee, or commonly it is described as feeling it is “under the knee cap”. It can be described as more of an aching type pain that is made worse on repetitive activities like running, going up or down stairs or prolonged sitting with the knee bent.
So Why Can PFPS Develop?
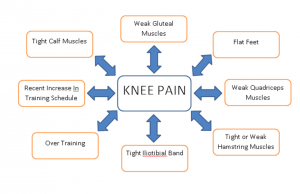
As is demonstrated by the diagram, there are many reasons that account for developing PFPS. A common reason is weakness of the quadriceps muscles and in particular the Vastus Medialis Oblique (VMO), allowing an increased pull from the vastus lateralis, ITB and lateral retinaculum to displace the knee cap laterally. Although PFPS is a knee pathology it isn’t just at the knee where problems occur resulting in the development of the condition. Weakness to the gluteal muscles allows an excessive amount of internal rotation of the femur placing higher demands on the knee cap and the knee joint. Similarly over pronation of the feet (known as being flat footed) can cause increased internal rotation at the knee which has a double effect of irritating the knee but also inhibiting the gluteal muscles. So it is easy to see why foot position plays a big part in PFPS. Other factors responsible for developing PFPS include tightness of the hamstrings and gastrocnemius muscles, as when they are tight they cause an increase in knee flexion with creates greater forces through the knee potentially irritating the back of the knee cap.
How Can PFPS Be Treated?
PFPS can be treated successfully by your physiotherapist. It is important to have a thorough assessment in order to work out exactly what biomechanical factors are causing your knee pain. Once this is established a treatment plan can be implemented. Initially treatments can be aimed at reducing pain and then correcting the biomechanical issues. To begin with rest is encouraged as it helps to unload the knee joint and reduce the amount of irritation occurring. Various physiotherapeutic techniques may be used such as; mobilisations to the knee cap, deep soft tissue massage and myofascial release to the muscles around the knee, taping to unload the knee and ice. As PFPS is usually related to biomechanical dysfunction there is a rehabilitation component to the recovery also. This usually involves strengthening of the quadriceps and gluteal muscles, stretching to tight structures i.e. ITB or hamstrings and assistance with returning to sport. Your physiotherapist will help you to formulate a programme that is both appropriate and specific to your individual needs. If the assessment reveals a biomechanical fault at the feet, you can be referred to a biomechanical specialist in order to have your gait analysed in great detail and then have some orthotic insoles cast to match your exact foot shape in order to help correct the fault.
Prognosis
PFPS generally has a positive outcome. It can however take anywhere between several weeks to a few months to resolve depending on what structures are involved and how well the rehabilitation goes and the extent of the injury in the first place.
Patella Tendinopathy
Patella tendinopathy is a bit of an umbrella term used to define pain and dysfunction to the patella tendon. It may be called “tendonitis” by some reference sources but this is not strictly accurate as this suggests that there is an inflammatory aspect to the problem underlying the condition which is not the case.
It is traditionally known as a condition to affect jumpers but it may also affect athletes of any variety of sports. It is usually caused by repetitive overload to the tendon.



