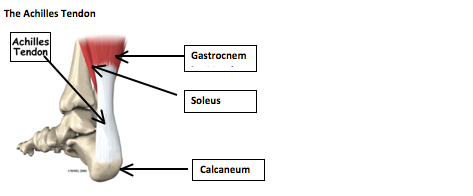
The Achilles Tendon
SymptomsThe Achilles tendon is a strong tendon that is formed from the Gastrocnemius Muscle (the large bulky muscle of the calf) and the Soleus Muscle (the smaller lower muscle of the calf); it attaches these muscles onto the Calcaneus (heal bone). These calf muscles contract and point the foot downwards; this allows one to stand on tip-toes, walk, run and jump. It is the strongest tendon of the body and can be subject to 3 times body weight whilst running.
Specific Risk factors for Achilles Tendinopathy in Runners
- Previous Achilles Tendinopathy
- Calf muscle tightness
- Over training on hard terrain
- Poor foot biomechanics, especially a high arched foot.
- Presence of bunions
- Poor footwear
- Pain is normally in the middle portion of the Achilles; however it can also be anywhere along the length of the tendon from the junction of the muscle and tendon, all the way to the point where the tendon meets the heal bone.
- Swelling or nodules on the tendon.
- Morning stiffness when trying to place foot onto floor
- Pain during warm-up of an activity (e.g. running), easing as one continues, then large increase in pain within the 24 hours after running.
- Pain with walking down stairs
- Reducing calf strength
Physiotherapy Assessment
During a physiotherapy assessment, the therapist may ask a client to walk, run, go up and down stairs, and perform various functional assessments to see how the tendinopathy is affecting function and ability. This may be timed or counted and will be used by the physiotherapist to assess how well the client is progressing.
Orthopaedic Investigations
The medical investigation normally used to confirm diagnosis is an ultrasound scan. A consultant may request one to try to diagnose the stage of the condition as this can affect the rehabilitation.
REHABILITATION
This is a general programme that most physiotherapists will use and has been shown clinically to be effective and provide long term management. It is important to note that different physiotherapists may do things slightly differently however the goal is to return the client to their previous level of activity pain-free.
Another important note is that a client may not get 100% improvement from an Achilles tendinopathy. The reason for this is that (as explained during the initial article on tendinopathy) some of the processes that cause tendinopathy can involve degeneration of the collagen fibres in the tendon; depending on the amount of this degeneration a tendon’s integrity may not go back to 100%. This is why effective rehabilitation, cross training, strength training and reducing any modifiable risk factors are very important. Nonetheless a physiotherapist will do everything possible to provide a client with a rehabilitation programme to enhance the chance of 100% success and return to sport.
Early Phase Intervention
- Patient education on the condition, and what to do and not to do (e.g. stop squeezing the tendon and no stretching).
- Icing – 15 minutes at a time, every hour if possible.
- Activity modification. This involves avoiding any aggravating activities (e.g. running or prolonged walks).
- Maintaining cardiovascular fitness through cycling and swimming.
- Assess and alter footwear if required; this may include changing trainers, providing orthotics, or even giving a heal raise to fit in shoes that can reduce any stretching of the Achilles tendon.
- Bilateral Heal raise holds, progressing to single leg heal raise holds.
- Single leg standing to improve balance
- Taping to support the Achilles tendon and to reduce the risk of stretching the Tendon.
- Calf massage, enhanced by using a foam roller or a spikey ball.
- Manual therapy from the physiotherapist to improve any ankle joint stiffness that may be present.
- Addressing any strength deficits through rest of lower limb or core stability; this may involve squats, lunges, Pilates based exercises.
All exercises and activities should be pain-free during the exercise, should not increase pain over the 24 hours after doing the exercise, and should be ceased before fatigue occurs.
To progress to the mid-phase of treatment the client should have reduced pain from the Achilles tendon, be able to hold a heal raise with approximately 10kg for at least 1 minute, pain-free during and for the 24 hours post the exercise.
Mid-Phase of treatment
- Maintaining icing, activity modification and cardiovascular fitness.
- Continuation of Calf massage and manual therapy if needed
- Bilateral and single-leg through-range heal raises; this can be progressed further by increasing the speed, weight or repetitions.
- A dynamic exercise is stair-climbing on tip-toes.
- Continuation of general lower limb and core strengthening.
To progress to the end stage of treatment the client should have no pain, be able to single-leg heal-raise through range with at least 10kg and this is pain-free. A physiotherapist may also choose to ask a client to hop as high as they can or for as far as the can to see how well the Achilles tendon is performing.
Late Phase Treatment
- Gradual return to sport using appropriate periodised programme. If this is running, a “return-to-running” programme can be used; this often looks similar to this (days relate to training days):
- Day 1 – walk 20 minutes
- Day 2 – walk 4 minutes, run 1 minute; repeat 4 times to bring to the total time to 20 minutes.
- Day 3 – walk 3 minutes, run 2 minutes; repeat 4 times to bring to the total time to 20 minutes.
- Day 4 – walk 2 minutes, run 3 minutes; repeat 4 times to bring to the total time to 20 minutes.
- Day 5 – walk 1 minute, run 4 minutes; repeat 4 times to bring to the total time to 20 minutes.
- Day 6 – run 20 minutes.
- Day 7 – run 25 minutes.
- Day 8 – run 30 minutes.
- From this point onwards continue to increase run distance by 5 minutes until up to previous length of time run. Once up to a normal time, then reduce back to 20 minutes and increase the pace of the run; gradually increase the time by 5 minutes at this higher pace.
- The entire running programme should be pain-free, and the Achilles should be monitored throughout the run and for the 24 hours after it. The client must be strict about the timings no matter how good they are feeling; if the tendon is going to flare up, it is unlikely that it will be painful during the run, instead it will be painful over the forthcoming 24 hours. If this happens the rehabilitation programme will have to start from the beginning again.
- Incline running (running up a hill) should be the last thing that is added into any rehabilitation programme.
- Running specific drills; these could include stride throughs, hurdle work, hopping, skipping, bounding.
- Maintain cross training and icing.
- Continue to improvement of lower limb and core strength.
Conclusion
Hopefully this provides a general programme of what to expect when attending physiotherapy for an Achilles tendinopathy. As stated earlier each physiotherapist may do things slightly different and this is purely some guidance.
Any questions that you may have or if you would like further information please do not hesitate to contact the clinic.