The Shoulder
a) “Compression type” tendinopathy. The shoulder needs to have a large range of movement to enable the functional requirements of normal life, as well as the added pressures placed on it by athletes. This means that mechanically it compromises some of its structural stability; instead it relies heavily on the muscles around shoulder, chest, back and arm to work together to keep it in place and be efficient in carrying out tasks.
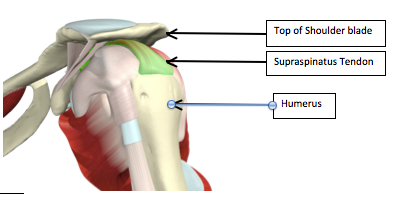
Most shoulder conditions and pain is caused when these muscles either do not work in sync, or some are overactive and others are underactive; this is especially true for shoulder tendinopathy. Shoulder tendinopathy usually affects the Supraspinatus tendon (green part of picture above); this is because it runs through a narrow gap between the top of the shoulder blade and the top of the humerus. This gap has other structures within it too, for example a fluid filled sac called a bursa. As the arm is taken above the head, the arm relies on a group of muscles called the Rotator Cuff to rotate to humerus so it clears the top of the shoulder blade.
Here are four types of tendinopathy, named (by me!), that are the most common in the shoulder. Notably they are not named by the tendon but rather by the cause.
– Firstly this can be caused if there is any osteoarthritic changes to the top of the shoulder blade; this reduces the small gap and can pinch the tendons between the humerus and shoulder blade. Like the other tendons discussed in this series, the supraspinatus tendon does not like being squashed and the tendon gets irritated, causing the sheath around the tendon to get inflamed; this increases the tendon’s size and then augments the likelihood of it getting pinched. This starts the cycle off again. If it continues the tendon itself can degenerate, increasing its susceptibility to tendinopathy.
– Secondly if the bursa gets irritated (often due to a sudden burst of activity eg DIY, lifting, painting), the bursa inflames and swells, and reduces the gap. This can happen separately or alongside the osteoarthritic changes. This causes the tendon to get pinched and irritated.
– Thirdly if the chest, arm, back or rotator cuff muscles are not working in sync then the humerus may not clear the shoulder blade well, and it can pinch the tendons (or the bursa)in the small gap.
b) “Altered pattern of movement” type tendinopathy.
– If one of the rotator cuff muscles, or some of the back, chest or arm muscles become overactive or underactive the synchronization between all these muscles alters (why this occurs is beyond the scope of this article). This either causes muscles to overwork and therefore increases the loading of tendons (predisposing to a tendinopathy as per other tendons), or it alters the ability of the rotator cuff muscles to clear the top of the scapula so causing a compression type tendinopathy.
c) “Weekend Warrior” type Tendinopathy
– This normally occurs because of a sudden burst of activity, for instance DIY, Overhead Painting or lifting. Like the other tendons dicussed in this series, the load required is beyond the capacity of the tendons or the muscles to cope. This then causes a tendinopathy (see main tendinopathy article for explanation of processes).
In summary there are multiple factors that can cause a shoulder tendinopathy. Physiotherapy will aim to modify these risk factors and alter patterns of movement to reduce the tendinopathy symptoms.
Specific Risk factors for a Shoulder Tendinopathy
– Poor posture
– Sudden increase in activity
– Increase in age
– Previous shoulder injury
– Lots of bench pressing or chest work in gym
– Prolonged sitting
Symptoms of a Shoulder Tendinopathy.
– Reduced shoulder strength
– Pain normally at the top of the arm or into the biceps muscles
– Pain at back of shoulder
– Pain when lying on shoulder
– Pain with activity, especially at horizontal.
– Occasional feeling of catching the arm.
– Neck or upper back pain
Physiotherapy Assessment
During a physiotherapy assessment, the therapist may ask a client to perform the most painful movement, lift the arms above the head, and perform various functional movements to see how the tendinopathy is affecting function and ability; during these functional tasks the therapist will also look at how the shoulder blade moves throughout the movement to establish if this could be adding to the problem. The therapist may then try to alter a part of this movement (ie change the client’s posture, shoulder blade movement, or angle of arm movement) to see if that affects the nature of the pain.
Lastly the therapist is likely to do a number of other tests to rule-out other pathologies that may mimic tendinopathy.
Orthopaedic Assessment
The medical investigation normally used to confirm diagnosis is an ultrasound scan. A consultant may request one to try to determine why the tendinopathy has occurred (ie to see if the bursa is inflamed, if there are degenerative changes of the tendon, or if there is some evidence of osteoarthritis). It may also be used to check there are no tears within the tendon or muscle that may account for the pain. If an ultrasound scan is not used then an MRI scan may be instead.
Rehabilitation
Rehabilitation is not broken down strictly in to early, mid and late stage as much as trying to correct the altered patterns of movement that have caused the tendinopathy.
1) Load management and patient education
– This involves stopping the aggravating movement as much as possible, for example not carrying a handbag on the affected side, or not doing bench pressing in the gym.
2) Scapula Control
– This may include taping to give the client feedback on where the correct scapular position is.
– Scapula exercises lying down, progressing to sitting and standing up, moving the arm through its range.
– Exercises that mimic the most painful functional movement.
– All these exercises will be painfree and fatigue free
3) Stretching of tight muscles
– These often include chest stretches or shoulder stretches.
4) Rotator cuff muscle strengthening
– This will be largely working on the synchronization of the shoulder muscles, especially the rotator cuff muscles. This will start with arm rotation exercises lying down, progressing to sitting up and standing up.
– Once these muscles are strong and synchronized then exercises will be started involving scapula movement and rotator cuff muscle strengthening. The purpose of this is to reduce the risk of the tendinopathy happening again.
5) Rectifying any other factors involved, for example neck pain, poor posture, back stiffness.
How this rehabilitation happens and the exercises given are very dependant on the therapist, what the client can do, and what the client wants to be able to do. This is a very general programme and different to the prescriptive nature of the others in this series.
Shoulder Tendinopathy Conclusion
Hopefully this provides a general programme of what to expect when attending physiotherapy for a shoulder tendinopathy. As stated earlier each physiotherapist may do things slightly different and this is purely some guidance.
Any questions that you may have or if you would like further information please do not hesitate to contact the clinic.